Posted: October 18th, 2021
6 most common soap note errors made by doctors.
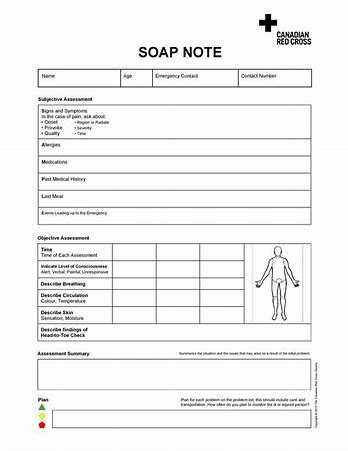
Soap Notes
Soap notes can be complex, but it is important that they are written well because this will help the nurse to provide better care for patients. Medical documentation is critical in medical records and the assessment of patients. So what are some common errors made when writing soap notes?
Abbreviations as soap note errors
The first type of error involves using too many abbreviations and acronyms; these may not mean anything to the nurses who are reviewing them. So if a doctor writes “SOAP ME,” this may be confusing to other health care providers.
Too much information soap note errors
Another common soap note error is when doctors write too much information in their notes, making it difficult for others to understand what they were trying to say; they often use run-on sentences and don’t provide enough information. So if the doctor writes, “the patient is a 67-year old male who comes in with complaints of chest pain that started about an hour ago,” this may not give nurses much to go on when trying to assess and treat patients.
Unclear notes
When writing soap notes, doctors need to make sure they are clear and concise; they should avoid using pronouns or vague words like “this” and “thing.” So if the doctor writes, “he has pain in this area,” this makes it difficult for nurses to determine what medical issues need to be addressed.
Too much information about oneself- healthcare providers
Another type of soap note error is when doctors write too much information about themselves; they should only include their name and the date at the top of each soap note. So if doctors write, “I saw this patient today,” nurses may not know what medical issues need to be addressed or how long patients will require treatment for; they also shouldn’t write about why they are seeing patients because it is considered unprofessional conduct.
Too little information in soap notes- pertinent medical history
Another type of soap note error is when doctors write too little information and don’t include any specific patient problems; they often forget to address why patients are in the hospital or what procedures will be performed while they are there. The patient’s chief complaint is not recorded. So if a doctor writes, “I saw this patient today,” nurses may not know whether patients require treatment for issues that are life-threatening or if they are there for routine checkups. Soap notes should address any conditions that could affect patient care and how long treatment will last. It is a critical component in the soap methodology and soap format.
Missing information, like time spent with the patient
Another type of soap note error is when doctors don’t include the time spent with patients in the subjective and objective sections; this makes it difficult for nurses to know whether appointments lasted longer than scheduled, which can affect patient care. So if the doctor writes, “I saw this patient today,” nurses may not know whether appointments lasted longer than scheduled or how long patients will require treatment for; they also shouldn’t write about why doctors are seeing patients because it is considered unprofessional conduct. Objective data goes missing and the progress notes have gaps.
Failing to explain why the patient is being discharged- surgical history
The last type of soap note error involves failing to explain why patients are being discharged; nurses may not know the procedures that need to be completed before they can leave. So if a doctor writes, “I saw this patient today,” nurses may get confused about whether patients require treatment for issues that are life-threatening or if they are there for routine checkups. Soap notes should address any conditions that could affect patient care and how long treatment will last. Soap notes can be complex, but it is important that they are written well because this will help the nurse to provide better care for patients. Case notes are a comprehensive assessment for patient care detailing the symptoms, radiological work, differential diagnosis, treatment plan, and the procedures performed on the patient.

Conclusion
Soap notes are an important part of medical history. They provide a clear, concise medical notes summary that is easy to read and understand by other healthcare providers. However, they can be time-consuming to write or difficult for some people who aren’t adept at writing in this style. If you need help with soap note summaries or any other aspect of your nursing career, let us know! Our team would love to partner with you on your next project so you get the recognition and results you deserve–from clinical services like soap note summaries all the way up to leadership positions within hospitals or clinics.”
Expert paper writers are just a few clicks away
Place an order in 3 easy steps. Takes less than 5 mins.
